Monitor claims and reduce costs
Incurring a loss is a stressful time because more often than not, you have never been through such an experience. UNICO’s Claims Advocates can lessen your stress by helping you through the whole process.


Proven results
In 2023, our Claim Advocacy and reserve verifications lowered claim reserves by over $4,400,000 resulting in almost $2,400,000 in premium saved due to decreases in their experience modification factor.
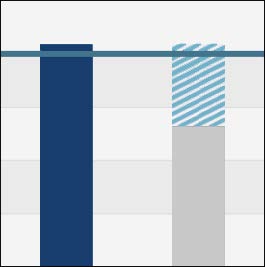
Mod premium analysis
The mod analysis graph highlights 4 key figures. Compare your current mod with the minimum mod to determine how much money you could be saving each year.
Work comp claim management examples:
In August before the insured’s data was reported to NCCI we did a mod projection which showed them that we expected their mod to go from a rate of 1.01 to a .97. In February the insured noticed at that time that their mod rate was 1.03 when we had projected it at .97
In reviewing the mod sheet the Claims Advocate determined that a previous policy period was not on the experience mod sheet. After working with the carrier and NCCI, the mod was lowered from the original 1.03 to a .92. The actual rate was even lower than the original projection due to January 1 rate changes.
Had the insured not known where their mod was projected they wouldn’t have ever questioned the higher rate and they would have likely lived with an incorrectly calculated high mod for the entire policy year.
While reviewing an experience mod worksheet for a client, it was noted that they had a claim for an individual on their mod which did not belong to the insured.
After much investigation we were able to determine that the claimant was employed by a third party which had no connection to the insured, but for some reason the state of Idaho/Chubb applied that claim to our insured.
This misfiled claim increased the mod by .0120 resulting in an additional annual premium to the insured of $5,999.
Claim management example:
Our insured mistakenly submitted an NEOC complaint for wrongful termination to their General Liability carrier who had $25k limits for EPLI coverage.
Once the GL carrier found that they had a primary EPLI policy with Philadelphia Insurance they tendered the claim to Philadelphia. This was four months after the complaint had been filed. UNICO got involved when the claim was over 2 years old and stepped in and worked directly with the adjuster to find out why reimbursement had not been made to our insured.
We found out that the carrier did not feel that they owed pretender attorney fees (attorney fees incurred prior to the notice of claim given to the carrier) based on their policy language. The carrier also had limits on the hourly fees charged by defense attorneys. We were able to successfully argue, based on case law, that they should be paid. We were also able to get the carrier to further review some of their decisions on what should and should not be paid and were able to get additional payment.
The whole process took 5 months of back and forth, working with both the insured and the carrier to find out what the carrier had communicated, getting the insured to provide records, and going up the chain of command to get the carrier to reconsider previous decisions, before finally getting reimbursement for the insured.
Additional services based on your needs
- Provide assistance and work collaboratively with client to accurately prepare claims documentation
- Address claim delays and move pending claims toward closure
- Address coverage or reserve issues
- Monitor activities of large claims and litigated claims
- Analyze claims data to determine loss trends and assist in loss prevention
- Attend and facilitate claim reviews, client meetings and vendor visits
- Assist the client in properly determining coverage